Throughout one’s life, it’s common to have health issues arise from time to time. While the medical system can be dysfunctional, it’s generally possible to seek and receive care for any particular issue. This is what people expect if they sustain a concussion. The reality is something entirely different.
It’s a shock to find that the diagnostic and treatment options are limited. The lack of technological advances and equipment has impacted treatment and recovery. The general approach for decades has been that if your concussion symptoms extend past a few weeks, it’s all emotion-based and you’re making everything up. This is highly destructive, to say the least. It also results in a lack of treatment options during recovery.
Historical Approach
The approach to identification and care has been inadequate. These are some of the issues.
- A study published by Ruff in 1996 became a roadmap followed by physicians in the years that followed. This study labeled concussees with PCS with a derogatory term I won’t use. It asserted that people were making things up, malingering, and often seeking to sue people. I believe that this has been the basis of care since that time. [1] [2]
- Visits to the emergency room (ER) often resulted in imaging tests, including CT and MRI scans. Both of those are known not to show concussion. [2]
- Little to no tech has been available. While advances are made in other health care situations [for example, taking one’s temperature], not much has occurred over decades for concussion.
Treatment options have been limited. That makes it difficult to identify issues and obtain treatment.
- Neuropsychological testing has been the main tool used. This is a combination of cognitive and psychological tests.
- Balance testing was and still is conducted using the BESS protocol. It’s a subjective, non-technical test where a person looks at a patient to see if they lost balance while in different positions. The use of technology such as force plates and sensors have been limited. This hampered identification of balance issues and proper treatment. I’m of the mind that the BESS should be discontinued and immediate steps taken to use force plates and sensors instead.
- Use of imaging options such as functional MRI (fMRI) and PET are available to researchers, but generally not to the public.
Recent Changes
In the past few years, the concussion topic has been overwhelmed and overrun by a focus on sports and CTE. While it has brought some attention to concussion issues, it has also harmed those who sustained non-sports concussions. There is a great difference between the two.
Because of the substantial differences in type of injury and effect on daily living due to life phase, different treatment options are warranted. This is a quick overview.
Mechanism of Injury
Sports: ongoing. There can be repeat concussions. Patients can be younger in age.
Motor vehicle accident (MVA): coup – contrecoup, whiplash, and generally a one-time occurrence. This skews more to adults.
Falls: One-time occurrence.
Life Changes
Sports (teens): impacts education (Return to Learn: RTL) and activities (Return to Play: RTP) Non-sports (adults): impacts employment (Return to Work: RTW) and family responsibilities
Use of Neuropsychology Reports by Insurance Companies
Neuropsychological reports have long been a foundation of concussion care. There are extensive tests that can take a full day and more. The baseline computer tests are a shortened version of the cognitive tests. The larger test series includes psychological questions. As far as I know, the baseline tests do not. Neuropsychological tests are very helpful and provide important information about cognitive issues that result from a concussion. However, there are issues with those tests.
One potential problem I see with neuropsychology tests, especially the baseline computer tests, is that I think the time of day the tests are taken are a factor. I believe that people tend to schedule appointments when they think they’d have the most energy. I know I did, which in retrospect I believe was a wrong approach. I think appointments and tests should occur when people will be at their worst regarding symptoms. It’s common to hit a wall at some point during the day, and then that might be it for the day. That’s when tests following concussions should be taken. That would provide a more accurate result, in my opinion. It’s the same for scheduling physician appointments. Schedule afternoon appointments or whenever symptoms are generally worse for you.
Physicians working for insurance companies review the neuropsychology reports. They weaponize the reports and use them against patients to deny claims. No matter what other physical issues might be raised, the insurance companies focus on the neuropsychology reports. Because neuropsychologists follow the Ruff view (in my opinion), malingering and supposed motives regarding lawsuits and other issues are seen as evidence that a person is not really experiencing physical issues.
I don’t know that neuropsychologists are aware of how their reports are used. The only way for patients to know is to request a copy of their insurance records. I did order a copy of mine and was shocked to find how reports were interpreted, the character attacks against me, and what information was overlooked.
This is why there needs to be more physical treatment options. It’s my opinion that it’s also time for neuropsychology to be at a lower level regarding treatment instead of a top, main level. I suggest evening it all out so all symptoms are at the same level, and whatever people experience rises to a higher level. (Ex: if experiencing tinnitus or hearing issues, see an audiologist. If having hormone issues, see an endocrinologist.)
Instead of claiming that everything is emotionally based, it’s time to refer patients to specialists who can address individual physical symptoms. No one would want to experience tinnitus or have their menstrual cycles put into disarray. What’s needed is to find the physical root cause of all these various symptoms. For too long, focus has been on emotional causes.
Regarding anxiety which is commonly mentioned as a cause of symptoms: life has many stressors, and more might surface following a concussion. For just one example, people’s employment might be affected. it’s stressful to lose a job. In fact, it’s recognized as a major life stressor. [3] [4] [5] I would think that experiencing an injury that results in the loss of job or career would contribute to having some anxiety. The physical issue and subsequent losses can lead to anxiety and emotional distress due to the loss. I think this is overlooked. That’s just one stressor.
Experiencing ongoing issues results in tremendous stress. Everyone I’ve come across just wants their lives and work back the way they were. Post-concussion existence is no glamour life. Why physicians think people are making things up for some imagined monetary reasons is mind-boggling. You lose far more income and benefits than you would ever gain otherwise. Losses can be substantial and affect your entire life. [6] This major disconnect is Grand-Canyonesque in its enormity, but sadly, not its grandeur. It should be reviewed.
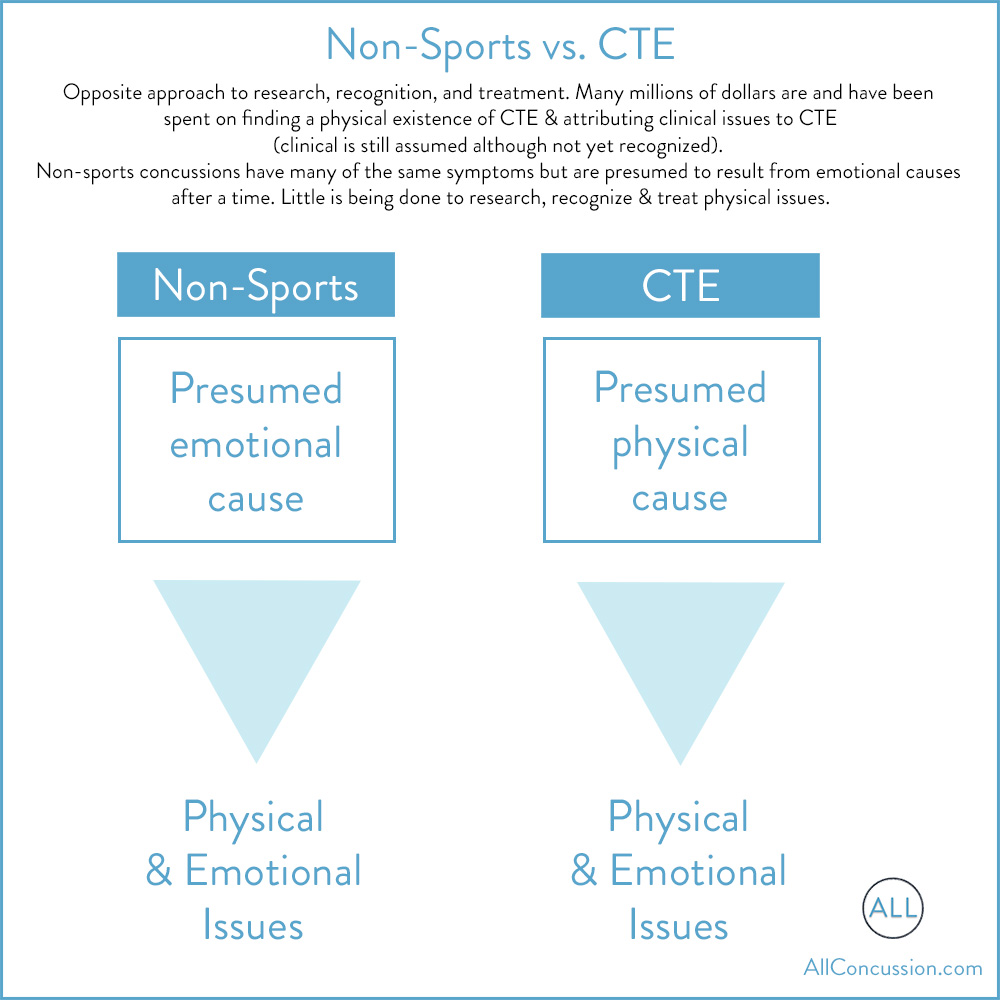
Non-Sports vs. CTE
Focus is on the physical existence of tau that results in CTE. Any clinical issues people have, including psychological, are attributed to the supposed physical cause of CTE. Millions upon millions of dollars are being applied to determining more about CTE. Research focuses on working from a physical standpoint (existence of tau). Researchers have found tau that is said to cause CTE, they’ve linked it to late-stage issues, and have been working to determine identifiable clinical indicators of CTE existence and progression. It’s being built from the ground up.
Conversely, focus for non-sports concussion remains on the complete opposite approach. This starts from the vantage point of presumed emotional issues over physical causes (if physical causes are even looked at).
A person who has sustained sports concussions and have physical and emotional symptoms: they and many in the medical community presume it’s all due to CTE. It’s presumed to be based on a physical cause. Those with non-sports concussion that have physical and emotional issues are presumed to have symptoms that emanate from emotional causes, not physical. This is a major disconnect that has had disastrous results and impact on non-sports concussees, particularly adults. Non-sports concussees constantly battle to obtain recognition and treatment for physical issues following a concussion.
Studies for CTE look for and support clinical symptoms and claim physical tau deposits are the root cause of all symptoms. Studies for non-sports focus more on emotional issues which are deemed to be the root cause. The concussee is blamed for supposedly causing physical issues due to emotional issues, anxiety, malingering, and a plan to engage in litigation.
Another irony in these two approaches is that CTE is a foundational issue for sports concussion lawsuits. For non-sports concussees, a supposed focus on lawsuits is used to dismiss ongoing symptoms and blame people for said symptoms.
For non-sports concussions, not as much is being spent on addressing the many physical symptoms that can result. There are also some crossover symptoms with post-concussion syndrome (or whatever it’s being referred to today) and CTE, but CTE people have been asserting that they’re different.
Sports vs. Non-Sports
No other health concern is subjected to this division of care. Think for a moment about other situations: heart conditions, asthma, cancer, anything else you can think of – are any of those divided into sports vs. non-sports? Are substantial monies and interest directed at sports only? The answer is a resounding “no.”
Those with other health conditions are also spared the constant call for body part donations. Nor do they have to see or try to avoid disturbing imagery. Have you seen images of hearts sliced into pieces and displayed on a table with researchers standing in front of them? How about lungs? Sounds odd, doesn’t it. Yet that is normal in the concussion and TBI world. How about seeing hearts or lungs in jars while researchers pose nearby? You just don’t see it. Yet, it’s the norm in the concussion and TBI world. It’s like living in a non-stop horror movie.
While I understand that researchers need to do their work and that they can review sliced up body parts objectively, I simply cannot. To me, that’s a person. It’s a major reason I won’t donate my brain or any other body part for research. Noone’s going to carve up parts of me and set said parts out for display for a photo op.
Next Steps
Here are a few ideas.
- It’s time to take non-sports concussions seriously and give them the same focus and research funding used for CTE.
- Flip the current approach to non-sports concussions and PCS to focus on physical issues. Use the approach taken currently for CTE: physical issue drives everything. Your brain runs your entire body. If you sustain an injury and have varied physical symptoms, why are said symptoms not addressed first?
- Call in outside experts that focus on the varied symptoms that concussees experience. It’s time to go outside the current setup, as that has failed too many people for far too long. It’s time to have specialists take a look so advancements can be made. Additional opinions can only help move treatments forward. Fast-track research and tech developments for non-sports concussions. The more people looking at this can only benefit everyone.
- I think that concussees need to also look outside current treatment options and see specialists for whatever physical symptoms you’re having. The current focus on emotional issues just isn’t enough. Decades of this approach haven’t worked. It’s time for something new.
That’s all I have for the moment. To non-sports concussees in particular: hang in there! Never give up…
[1] Ruff RM, Camenzuli L, Mueller J Miserable minority: emotional risk factors that influence the outcome of a mild traumatic brain injury 1996
[2] Shenton ME, Hamoda HM, Scheniderman JS, et al A review of magnetic resonance imaging and diffusion tensor imaging findings in mild traumatic brain injury 2012
[3] Holmes TH, Rahe Richard H The Social Readjustment Rating Scale 1967
[4] Holmes-Rahe Life Stress Inventory American Institute of Stress, stress.org
[5] The Toll of Job Loss American Psychological Association, October 1, 2020
[6] Norris J Income Loss Due to Concussion AllConcussion.com June 14, 2022